What is a Phalanx Fracture?
Kids are active, but not always graceful! Falls happen to children of all ages, and when they land on their outstretched hand or wrist, injuries can occur. Unfortunately, fractures are a right-of-passage for most children. Fractures are simply breaks or cracks in the bone. If they’ve already had an x-ray, and you’ve been told the bone was “broken”, “hairline”, “green stick”, “buckled”, “cracked”, “chipped”, “split”, “shattered”, or “splintered”, these are all just different ways of describing a fracture. Because children’s bones are more flexible than adults’, sometimes they “bend” or “buckle” like a “green stick” rather than cracking. Often the fractures occur around the soft growth plates at the wrist and bases of the fingers.
 X-ray Showing a Phalanx Fracture
X-ray Showing a Phalanx Fracture
Causes
Most causes of phalanx fracture involve trauma to the fingers:
- Sudden “jamming” injuries to the fingers (mallet fractures)
- Twisting or hyperextension injuries (dog leashes, falls, sports)
- Blunt force trauma (work injuries, sports, vehicle accidents)
- Hand crush injuries
- Enchondroma (benign bone cyst that weakens the bone until it fractures)
Signs and Symptoms
Symptoms of a phalanx fracture usually include one or more of the following:
- Finger pain and tenderness
- Finger swelling / stiffness
- Finger bruising
- Finger deformity (crooked fingers, end of finger won’t straighten)
Is There a Test for Phalanx Fractures?
Yes! Often fractures are obvious on physical examination, but severe sprains and contusions can also look and feel very much like a phalanx fracture. X-rays usually offer definitive diagnosis and help with treatment planning.
Treatment
Suspected hand fractures warrant emergent treatment if you are experiencing hand numbness and tingling, severe or “tight” swelling, significant deformity of the hand or any open wounds around the hand (possible open or compound fracture). Even without these warning signs, it is best to seek urgent treatment as the results of delayed treatment of phalanx fractures can lead to undesirable outcomes such as nonunion (won’t heal) or malunion (heals crooked).
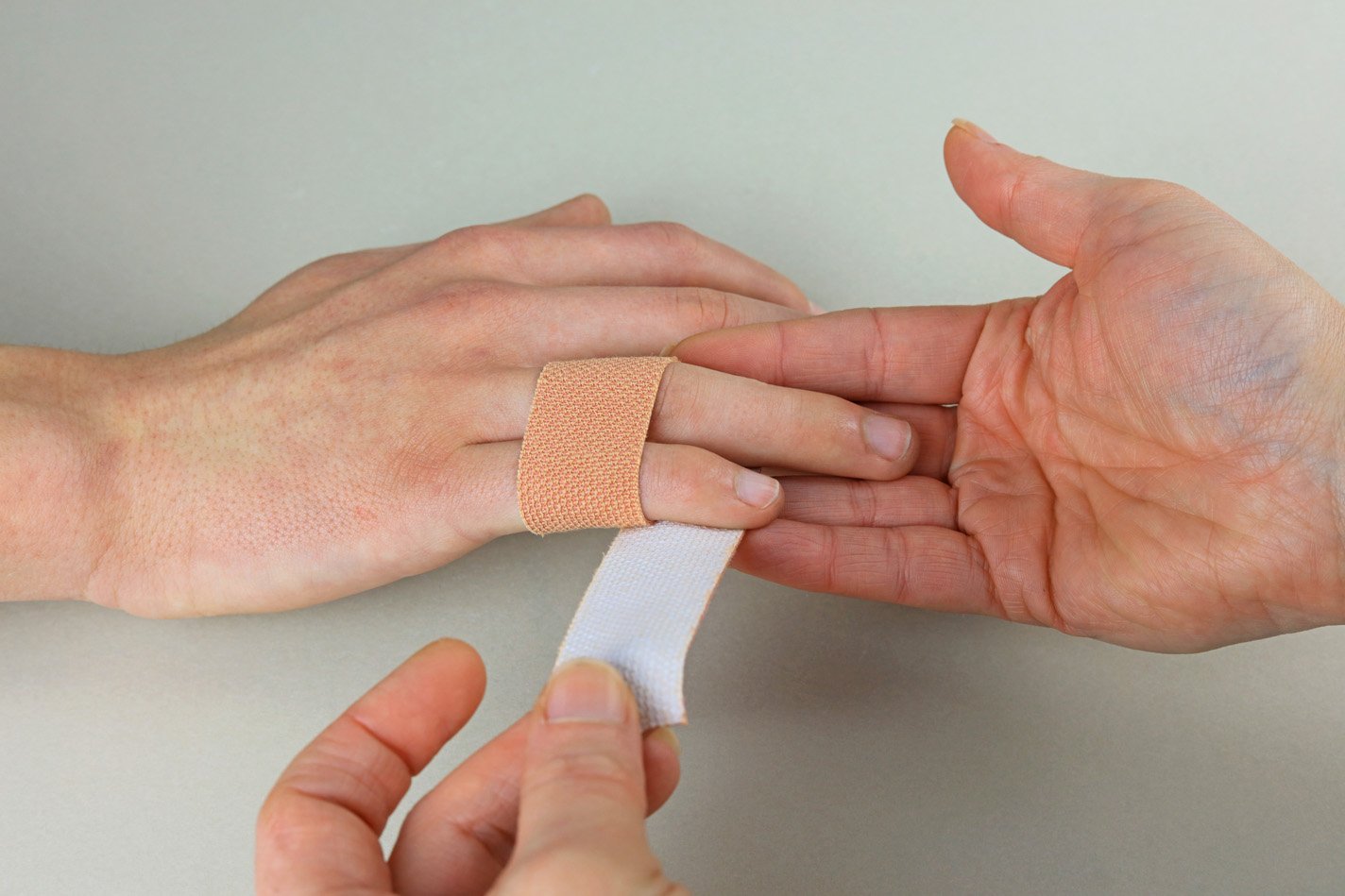
Nonoperative Treatment:
Splinting and buddy taping are the mainstays of nonoperative treatment for phalanx fractures. For many fractures, we start some early gentle motion, sometimes with Hand Therapy, to prevent permanent stiffness, but always follow the direction of your surgeon when it comes to moving or stretching a broken finger.
Operative Treatment:
Surgical repair of phalanx fractures is required when the fracture pieces are unstable (won’t stay in place), or not healing properly with splint treatment. Mild sedation is given, and a local block numbing of the finger is performed in the operating room. If the phalanx can be set straight, metal wires are placed through the skin and into the bone to keep it straight while it is healing. If the fracture is severe, it may be necessary to make a small incision over the finger to restore the alignment of the broken phalanx directly and hold the pieces in place with tiny metal plate and/or screws. Often, a second surgery is performed after the bone has healed, in order to remove the plate and screws if they are bothersome under the skin or causing finger stiffness.
 X-ray showing pinning in a finger to repair a Phalanx Fracture
X-ray showing pinning in a finger to repair a Phalanx Fracture
Ready to confirm a diagnosis and fix the problem or just want to learn more?
Our board-certified orthopedic hand and wrist surgeons Eric Angermeier, MD and Kyle Kokko, MD, PhD, are here to help! They can often diagnose the problem in one visit, and get you started with a treatment plan. We offer a wide variety of both nonoperative and operative treatment options.
Call today for a clinic or telehealth appointment! 854-429-4263